Obesity: Questions & Answers
Q1: Why did the American Medical Association (AMA) classify obesity as a disease in 2013?
A: The AMA recognized obesity as a disease because it is long-term, has many causes, involves changes in how the body regulates weight, and leads to serious health risks. Labeling it a disease helps reduce stigma and ensures patients get proper medical care.
Q2: What causes obesity?
A: Obesity has no single cause. It can result from:
Genetics (family history)
Hormonal and metabolic changes
Lifestyle factors (diet, physical activity, sleep)
Environmental influences (easy access to unhealthy foods, sedentary jobs)
Psychological factors (stress, emotional eating)
Often, several of these factors combine.
Q3: What health risks are linked to obesity?
A: Obesity increases the risk of many health problems, including:
Type 2 diabetes
High blood pressure and heart disease
Stroke
Sleep apnea
Certain cancers (such as breast, colon, and uterine cancer)
Joint pain and arthritis
Q4: How is obesity treated?
A: Treatment usually involves a long-term plan, which may include:
Healthy eating and physical activity
Behavioral support (counseling, stress management)
Medications to help with weight loss
Surgery (such as bariatric surgery) for certain patients
The best plan is personalized and guided by a healthcare professional.
Q5: Is obesity just a lifestyle problem?
A: No. While lifestyle choices play a role, obesity is not simply a matter of willpower. It is a medical condition influenced by biology, environment, and behavior. Recognizing it as a disease helps shift the focus from blame to treatment and support.
Diabetes: Questions & Answers
Q1: What is diabetes?
A: Diabetes is a chronic condition where the body has trouble using sugar (glucose) for energy. This happens because the body doesn’t make enough insulin or doesn’t use insulin properly. As a result, blood sugar levels stay too high.
Q4: What health risks are linked to diabetes?
A: Uncontrolled diabetes can lead to:
Heart disease and stroke
Kidney damage
Vision loss
Nerve damage (neuropathy)
Poor wound healing and foot problems
Q2: What are the types of diabetes?
A
Type 1 diabetes – The body makes little or no insulin. Usually starts in childhood or young adulthood.
Type 2 diabetes – The body doesn’t use insulin well. This is the most common type, often linked to weight, age, and family history.
Gestational diabetes – Develops during pregnancy and usually goes away after birth, but increases future risk of type 2 diabetes.
Q5: How is diabetes managed?
A: Management focuses on keeping blood sugar in a healthy range. This may include:
Healthy eating and regular physical activity
Blood sugar monitoring
Medications or insulin
Regular checkups to prevent complications
With proper care, people with diabetes can live long and healthy lives.
Q3: What symptoms should I watch for?
A: Common symptoms include:
Increased thirst and urination
Unexplained weight loss
Fatigue
Blurred vision
Slow-healing wounds or frequent infections
Sometimes type 2 diabetes develops silently with no early symptoms.
Hypertension: Questions & Answers
Q1: What is hypertension?
A: Hypertension means consistently high blood pressure in the arteries. It forces the heart to work harder to pump blood and, if untreated, can damage blood vessels and organs.
Q4: What health risks are linked to hypertension?
A: If uncontrolled, hypertension can lead to:
Heart attack and heart failure
Stroke
Kidney disease
Vision loss
Vascular dementia
Q2: Why is hypertension called the “silent killer”?
A: Most people with high blood pressure have no symptoms. It can quietly damage the heart, brain, kidneys, and eyes for years before problems appear, which is why regular checkups are important.
Q3: What causes hypertension?
A: Causes can include:
Genetics and family history
Aging
Excess salt in the diet
Being overweight or inactive
Smoking or heavy alcohol use
Stress
Medical conditions such as kidney disease or sleep apnea
Q5: How is hypertension treated?
A: Treatment usually combines:
Lifestyle changes (healthy diet, less salt, exercise, weight control, quitting smoking, limiting alcohol, managing stress)
Medications (if needed, often more than one)
Regular monitoring of blood pressure at home and with your doctor
With proper care, blood pressure can often be controlled for life.
High Cholesterol: Questions & Answers
Q1: What is cholesterol?
A: Cholesterol is a waxy substance found in your blood. Your body needs some cholesterol to build cells and make hormones. But too much cholesterol can build up in your arteries and increase your risk of heart disease and stroke.
Q4: What causes high cholesterol?
A: Causes include:
Genetics (family history)
Eating foods high in saturated and trans fats
Being overweight or physically inactive
Smoking
Medical conditions (like diabetes or hypothyroidism)
Aging (cholesterol levels often rise with age)
Q2: What does “high cholesterol” mean?
A: High cholesterol means your blood has too much LDL (“bad”) cholesterol or not enough HDL (“good”) cholesterol. LDL can form plaque in the arteries, while HDL helps remove cholesterol from the bloodstream.
Q3: What health risks are linked to high cholesterol?
A: Over time, high cholesterol can lead to:
Heart attack
Stroke
Peripheral artery disease
Narrowing of arteries (atherosclerosis)
Q5: How is high cholesterol treated?
A: Treatment usually includes:
Healthy lifestyle – heart-healthy diet, exercise, weight management, quitting smoking
Medications – such as statins or other cholesterol-lowering drugs if lifestyle changes aren’t enough
Regular monitoring – blood tests to track cholesterol levels
Depression: Questions & Answers
Q1: What is depression?
A: Depression is more than just feeling sad. It’s a medical condition that affects mood, thinking, energy, and daily life. It can last weeks to months or longer and often needs treatment.
Q3: What causes depression?
A: Depression has many causes, including:
Biological: Chemical imbalances in the brain, hormones, genetics
Psychological: Past trauma, stress, negative thought patterns
Social: Loneliness, loss, relationship or financial difficulties
Usually, it’s a combination of these factors.
Q2: What are the symptoms of depression?
A: Symptoms may include:
Feeling sad, empty, or hopeless most of the time
Loss of interest in activities once enjoyed
Changes in sleep (too much or too little)
Changes in appetite or weight
Fatigue or low energy
Difficulty concentrating or making decisions
Thoughts of death or suicide (in severe cases)
Q4: Why is depression serious?
A: Untreated depression can affect work, school, and relationships. It increases the risk of substance use, chronic illness, and suicide. But with treatment, most people improve and regain quality of life.
Q5: How is depression treated?
A: Treatment may include:
Therapy: Talking with a mental health professional
Medications: Antidepressants to balance brain chemicals
Lifestyle changes: Regular exercise, healthy sleep, social support
Severe cases: Hospital care, or specialized treatments like ECT or TMS
Help is available, and recovery is possible.
Insomnia: Questions & Answers
Q1: What is insomnia?
A: Insomnia is a sleep disorder where people have trouble falling asleep, staying asleep, or waking up too early and not being able to go back to sleep. It can be short-term (a few days or weeks) or chronic (lasting months or longer).
Q4: Why is insomnia serious?
A: Poor sleep affects health, safety, and quality of life. Long-term insomnia can increase the risk of:
High blood pressure, diabetes, and heart disease
Depression and anxiety
Weakened immune system
Poor concentration, memory, and workplace or driving accidents
Q2: What are the symptoms of insomnia?
A: Symptoms include:
Difficulty falling asleep at night
Waking up often during the night
Waking up too early in the morning
Feeling tired, irritable, or unfocused during the day
Relying on caffeine or naps to get through the day
Q5: How is insomnia treated?
A: Treatment often includes:
Sleep hygiene: Regular bedtime, limiting caffeine/alcohol, reducing screen time, creating a quiet and dark sleep environment
Cognitive Behavioral Therapy for Insomnia (CBT-I): A proven therapy that addresses thoughts and habits that interfere with sleep
Medications: Sometimes used short term if needed
Managing underlying conditions: Treating pain, anxiety, or other medical issues that disrupt sleep
Q3: What causes insomnia?
A: Causes may include:
Stress or anxiety
Poor sleep habits (irregular schedule, screen use at night, caffeine or alcohol late in the day)
Medical conditions (chronic pain, asthma, reflux, depression, etc.)
Medications (stimulants, steroids, some antidepressants)
Shift work or jet lag disrupting the sleep-wake cycle
Smoking: Questions & Answers
Q1: Why is smoking harmful?
A: Smoking damages nearly every organ in the body. Tobacco smoke contains thousands of chemicals, many of which are toxic and cancer-causing. It greatly increases the risk of cancer, heart disease, stroke, and lung diseases like COPD.
Q4: Are “light” cigarettes, e-cigarettes, or vaping safer?
A: There is no safe tobacco product. “Light” or low-tar cigarettes are still harmful. E-cigarettes and vaping may expose users to fewer toxins than smoking but still contain addictive nicotine and other harmful chemicals. More research is ongoing about long-term risks.
Q2: What health problems are linked to smoking?
A: Smoking can cause:
Lung cancer and many other cancers (mouth, throat, bladder, kidney, pancreas)
Heart disease and stroke
Chronic bronchitis and emphysema (COPD)
Weakened immune system
Infertility and pregnancy complications
Early aging of the skin and teeth problems
Q5: How can I quit smoking?
A: Quitting is hard but possible. Effective strategies include:
Behavioral support: Counseling, support groups, quit lines
Medications: Nicotine replacement (patches, gum, lozenges) or prescription drugs that reduce cravings
Lifestyle changes: Avoiding triggers, stress management, regular exercise
Professional help: Doctors, pharmacists, and smoking cessation programs can provide guidance and support
Even if you’ve tried before, each attempt increases the chance of success.
Q3: Why is nicotine addictive?
A: Nicotine, the main drug in tobacco, quickly reaches the brain and creates a temporary sense of pleasure or stress relief. Over time, the brain craves nicotine, leading to dependence and withdrawal symptoms when a person tries to quit.
Marijuana (Cannabis): Questions & Answers
Q1: What is marijuana?
A: Marijuana, also called cannabis, comes from the Cannabis plant. It contains THC (tetrahydrocannabinol), the chemical that causes a “high,” and CBD (cannabidiol), which does not cause intoxication but may affect the brain and body.
Q4: What are the risks of regular marijuana use?
A: Long-term or heavy use can lead to:
Dependence or addiction (cannabis use disorder)
Memory and learning problems
Decline in attention, especially in teens and young adults
Lung irritation (if smoked)
Mental health problems (higher risk of anxiety, depression, or psychosis in vulnerable individuals)
Q2: How is marijuana used?
A: Marijuana can be smoked, vaped, eaten (edibles), or used as oils or tinctures. The effects vary depending on how it’s taken.
Q5: Is marijuana safe or legal?
A: Marijuana laws vary by state. Some allow medical or recreational use; others prohibit it. Even where legal, marijuana is not risk-free. It can impair driving, affect mental health, and interact with other medications. Pregnant and breastfeeding women should avoid it, as it can affect babies’ brain development.
Q3: What are the short-term effects?
A:
Euphoria (“high”), relaxation
Altered senses (seeing or hearing things differently)
Increased appetite (“munchies”)
Poor coordination and slowed reaction time
Trouble with memory and concentration
Anxiety or paranoia in some users
Alcohol Use Disorder: Questions & Answers
Q1: What is alcohol use disorder (AUD)?
A: AUD is a medical condition where a person has trouble controlling or stopping alcohol use, even when it causes problems in health, work, or relationships. It ranges from mild to severe and is sometimes called alcohol dependence or alcoholism.
Q4: Why is alcohol use disorder serious?
A: AUD can cause major health and life problems, including:
Liver disease (fatty liver, cirrhosis)
Heart disease, high blood pressure, and stroke
Increased risk of cancers (mouth, throat, liver, breast)
Depression, anxiety, and memory problems
Accidents, injuries, and relationship breakdowns
Risk of alcohol poisoning and death in severe cases
Q2: What are the symptoms of alcohol use disorder?
A: Common signs include:
Drinking more or longer than intended
Unsuccessful attempts to cut down or stop
Spending a lot of time drinking or recovering from it
Strong cravings for alcohol
Continuing to drink despite health, relationship, or job problems
Needing more alcohol to get the same effect (tolerance)
Withdrawal symptoms when not drinking (shaking, sweating, anxiety, nausea)
Q5: How is alcohol use disorder treated?
A: Treatment depends on severity and may include:
Counseling and support: Cognitive Behavioral Therapy, group therapy, or 12-step programs (like Alcoholics Anonymous)
Medications: Naltrexone, acamprosate, or disulfiram to reduce cravings or prevent relapse
Medical detox: For safe withdrawal if alcohol use is heavy
Lifestyle and social support: Family support, stress management, and healthy routines
Recovery is possible, and many people live fulfilling lives after treatment.
Q3: What causes alcohol use disorder?
A: Causes are a mix of:
Biological factors: Genetics and brain chemistry
Psychological factors: Stress, trauma, or mental health conditions
Social factors: Peer pressure, easy access to alcohol, cultural influences
Not everyone who drinks develops AUD, but certain risk factors increase the chance.
Medication Abuse: Questions & Answers
Q1: What is medication abuse?
A: Medication abuse happens when prescription or over-the-counter (OTC) drugs are used in a way other than prescribed. This can mean taking higher doses, using someone else’s medication, or using it to get “high.”
Q4: Why is medication abuse dangerous?
A: Misusing medicines can cause:
Addiction and dependence
Overdose (sometimes life-threatening)
Damage to liver, kidneys, heart, or brain
Dangerous interactions with alcohol or other drugs
Accidents, poor judgment, and legal consequences
Q2: What types of medications are commonly abused?
A: The most commonly misused medicines are:
Pain relievers (opioids): oxycodone, hydrocodone, morphine
Anti-anxiety medicines and sedatives: benzodiazepines (Xanax, Valium)
Stimulants: ADHD medications like Adderall or Ritalin
Cough medicines: those containing dextromethorphan (DXM)
Q5: How can medication abuse be prevented or treated?
A:
Prevention: Take medicines only as prescribed, never share them, and store them safely.
Treatment: Counseling, behavioral therapies, support groups, and medications (such as for opioid addiction) can help.
Medical help: Doctors and addiction specialists can guide safe recovery.
Q3: Why do people misuse medications?
A: Reasons can include:
Trying to relieve pain, stress, or anxiety without medical guidance
Seeking improved focus, energy, or weight loss
Using to get high or to escape problems
Peer pressure or social influence
Cancer Screening for Women: Questions & Answers
Q1: Why is cancer screening important?
A: Screening detects cancers early, often before symptoms appear. Early detection makes treatment more effective and can prevent cancer from progressing.
Q3: Are there other important screenings for women?
A: Yes.
Bone density test (DEXA scan): Recommended at age 65+ (earlier if risk factors for osteoporosis)
Genetic testing (BRCA, others): If strong family history of breast, ovarian, or uterine cancer
Q2: Which cancers should women over 45 be screened for?
A:
Breast cancer:
Mammogram every 1–2 years starting at age 40–45
Annual screening may be chosen based on personal risk factors
Cervical cancer:
Ages 21–65: Pap smear every 3 years
Ages 30–65: Pap smear + HPV test every 5 years (preferred)
Colorectal cancer:
Start at age 45
Colonoscopy every 10 years, or stool-based tests every 1–3 years
Lung cancer:
Annual low-dose CT scan for women age 50–80 with a 20+ pack-year smoking history, and who currently smoke or quit within the past 15 years
Skin cancer:
Skin checks, especially if high sun exposure or family history
Q4: What are the risks of screening?
A: Some tests may cause discomfort, false positives, or overdiagnosis (finding slow-growing cancers that might never cause harm). That’s why it’s important to discuss screening schedules with your doctor.
Q5: What else should women do for prevention?
A:
Stay up to date on vaccines (flu, shingles, pneumococcal, COVID-19, Tdap)
Get regular blood pressure, cholesterol, and diabetes checks
Maintain a healthy diet, exercise, and avoid smoking
Practice safe sun protection and routine skin checks
Cancer Screening for Men (50+): Questions & Answers
Q1: Why is cancer screening important?
A: Screening finds cancer early, often before symptoms start. Early detection makes treatment easier and more effective, and can even prevent some cancers from developing.
Q3: What about other cancers?
A: Depending on risk factors, men may also need:
Liver cancer screening if chronic hepatitis B or cirrhosis is present
Q2: Which cancers should men over 50 be screened for?
A:
Colorectal cancer:
Screening starts at age 45
Colonoscopy every 10 years, or stool-based tests every 1–3 years depending on type
Prostate cancer:
PSA (prostate-specific antigen) blood test discussed with your doctor starting at age 50
High-risk men (African American or strong family history) may start at 45
Lung cancer:
Annual low-dose CT scan for men age 50–80 with a 20+ pack-year smoking history, and who currently smoke or quit within the last 15 years
Skin cancer:
Periodic skin checks, especially for those with high sun exposure or family history
Q4: Are there risks with screening?
A: Yes. Some tests may cause discomfort, false positives, or overdiagnosis (finding cancers that would not have caused harm). That’s why shared decision-making with your healthcare provider is important.
Q5: What else should men over do for prevention?
A:
Stay up to date on vaccines (flu, shingles, pneumococcal, Tdap, COVID-19)
Routine blood pressure, cholesterol, and diabetes checks
Maintain a healthy weight, diet, and exercise routine
Avoid tobacco and limit alcohol use
Migraine: Questions & Answers
Q1: What is a migraine?
A: A migraine is more than just a headache. It’s a neurological condition that causes severe, throbbing head pain, often on one side, and is usually accompanied by other symptoms like nausea, sensitivity to light, or visual changes.
Q4: When are migraines serious?
A: While most migraines are not life-threatening, you should seek immediate care if a headache is sudden and severe (“thunderclap headache”), or comes with vision loss, weakness, confusion, or difficulty speaking. These may signal another serious condition, not a migraine.
Q2: What are the symptoms of a migraine?
A: Migraines can include:
Intense, throbbing head pain (often one-sided)
Nausea and vomiting
Sensitivity to light, sound, or smells
Visual disturbances (flashes, zigzag lines, blind spots—called “aura”)
Fatigue, brain fog, or mood changes before or after the headache
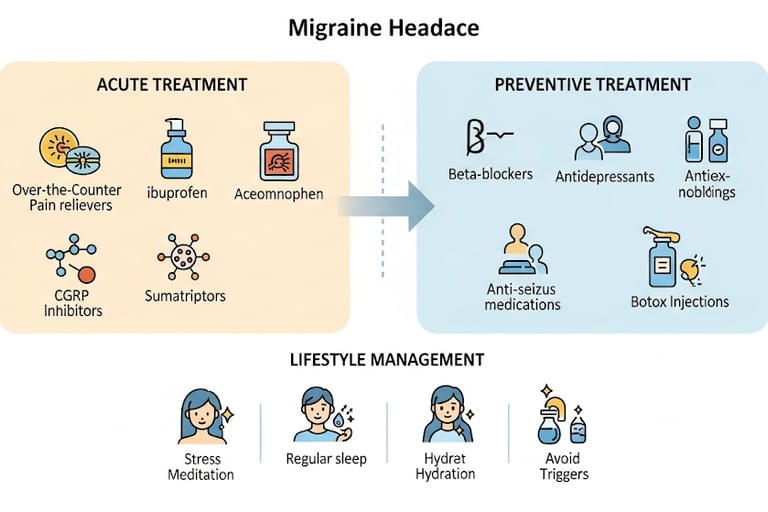
Q5: How are migraines treated?
A: Treatment focuses on relieving symptoms and preventing attacks:
Medications: Over-the-counter pain relievers, triptans, anti-nausea medicines, or preventive drugs for frequent migraines
Lifestyle changes: Regular sleep, stress management, hydration, avoiding known triggers
Other therapies: Biofeedback, relaxation training, acupuncture, or nerve stimulation devices (for some patients)
Q3: What triggers migraines?
A: Common triggers include:
Stress or lack of sleep
Hormonal changes (such as during menstruation)
Certain foods (aged cheese, processed meats, chocolate, caffeine changes)
Alcohol, especially red wine
Bright lights, strong odors, or loud noises
Weather changes or dehydration
Low Back Pain: Questions & Answers
Q1: What is low back pain?
A: Low back pain is discomfort or stiffness in the area between the lower ribs and the buttocks. It’s one of the most common medical problems and can be acute (lasting a few days to weeks) or chronic (lasting 3 months or longer
Q4: When should I see a doctor?
A: Most low back pain improves within a few weeks. Seek medical care if you have:
Severe pain that doesn’t improve with rest
Pain after a fall, accident, or injury
Numbness, tingling, or weakness in the legs
Trouble controlling bladder or bowels (medical emergency)
Fever, unexplained weight loss, or history of cancer
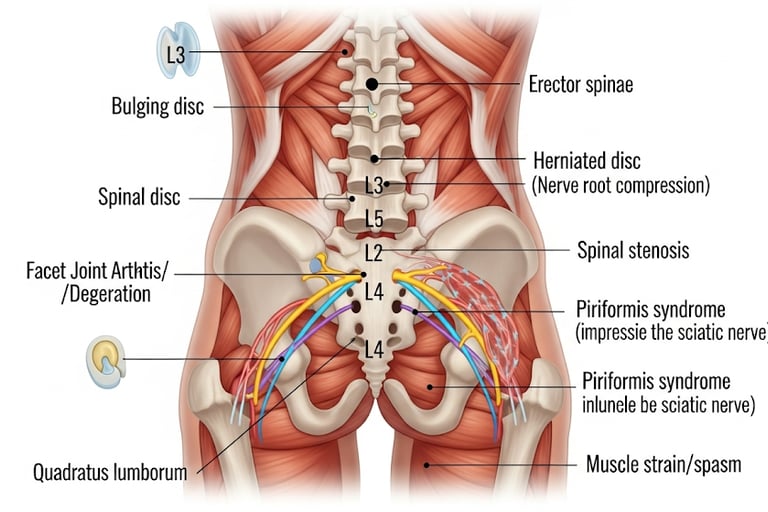
Q2: What causes low back pain?
A: Causes include:
Muscle or ligament strain (lifting heavy objects, sudden awkward movements)
Poor posture or prolonged sitting
Herniated or slipped disk
Arthritis or spinal stenosis (narrowing of the spinal canal)
Osteoporosis-related fractures
Less commonly, infection, tumors, or systemic illness
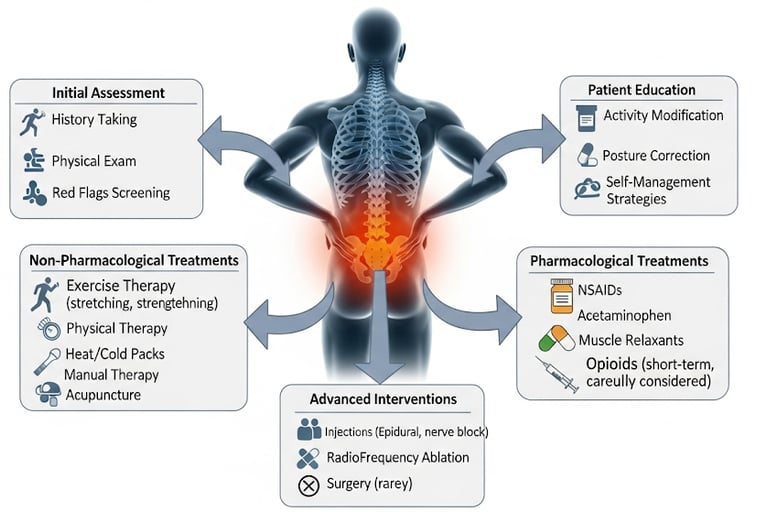
Q5: How is low back pain treated?
A: Treatment depends on the cause but often includes:
Self-care: Activity as tolerated, heat/ice, gentle stretching, over-the-counter pain relievers
Physical therapy: Exercises to strengthen muscles and improve posture
Medications: Anti-inflammatories, muscle relaxants, or nerve pain medicines
Injections: Steroids for inflammation near the nerves (in select cases)
Surgery: Rarely needed, only for severe structural problems or nerve compression
Q3: What are the symptoms?
A: Symptoms may include:
Aching, burning, or stabbing pain in the lower back
Pain that radiates into the buttock or leg (sciatica)
Stiffness or limited movement
Muscle spasms
Sometimes numbness, tingling, or weakness if nerves are involved
Arthritis: Questions & Answers
Q1: What is arthritis?
A: Arthritis is not just one disease—it’s a term for conditions that cause joint pain, stiffness, and swelling. The most common types are osteoarthritis (wear-and-tear on joints) and rheumatoid arthritis (an autoimmune disease where the immune system attacks the joints).
Q4: What problems can arthritis cause if untreated?
A: Without treatment, arthritis can lead to:
Chronic pain
Joint deformity or loss of function
Difficulty with daily activities (walking, climbing stairs, gripping objects)
Reduced quality of life
Q2: What are the symptoms of arthritis?
A: Symptoms can vary but often include:
Joint pain or stiffness (especially in the morning)
Swelling, warmth, or redness around joints
Limited movement or flexibility
Fatigue (especially in autoimmune forms like rheumatoid arthritis)
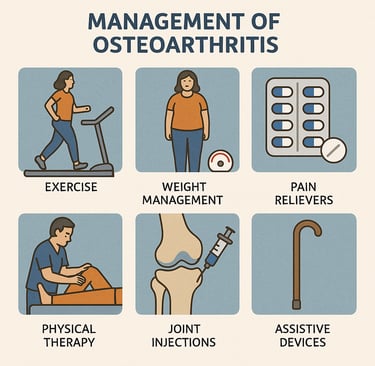
Q5: How is arthritis treated?
A: Treatment depends on the type, but may include:
Lifestyle changes: Regular exercise, healthy weight, joint protection techniques
Medications: Pain relievers, anti-inflammatory drugs, or immune-modifying drugs (for rheumatoid arthritis)
Physical therapy: To improve strength and mobility
Surgery: Joint repair or replacement in severe cases
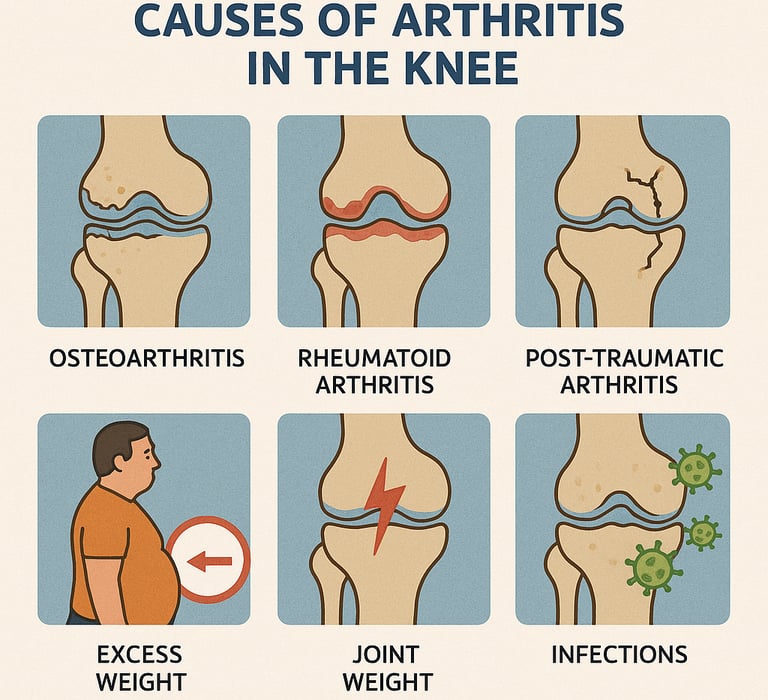
Q3: What causes arthritis?
A: Causes depend on the type of arthritis:
Osteoarthritis: Aging, joint overuse, injuries, and excess weight can wear down cartilage.
Rheumatoid arthritis: An autoimmune reaction where the body attacks its own joints.
Other causes: Infections, gout (uric acid buildup), or genetic factors

Adult Vaccines: Questions & Answers
Q1: Why are vaccines important for adults?
A: Vaccines protect adults from serious diseases and prevent spreading illness to others. Immunity from childhood shots can fade, and some vaccines are only given later in life. Staying up to date reduces the risk of severe infections, hospitalization, and complications.
Q4: Which vaccines are for specific risks?
HPV vaccine: Recommended through age 26; may be given up to age 45 based on risk factors
Hepatitis A and B vaccines: For adults at risk (travel, healthcare work, chronic liver disease, sexual exposure risks)
MMR (measles, mumps, rubella) and Varicella (chickenpox): If never vaccinated or lacking natural immunity
Meningococcal vaccine: For certain risk groups (college students, military recruits, or those with weak immune systems)
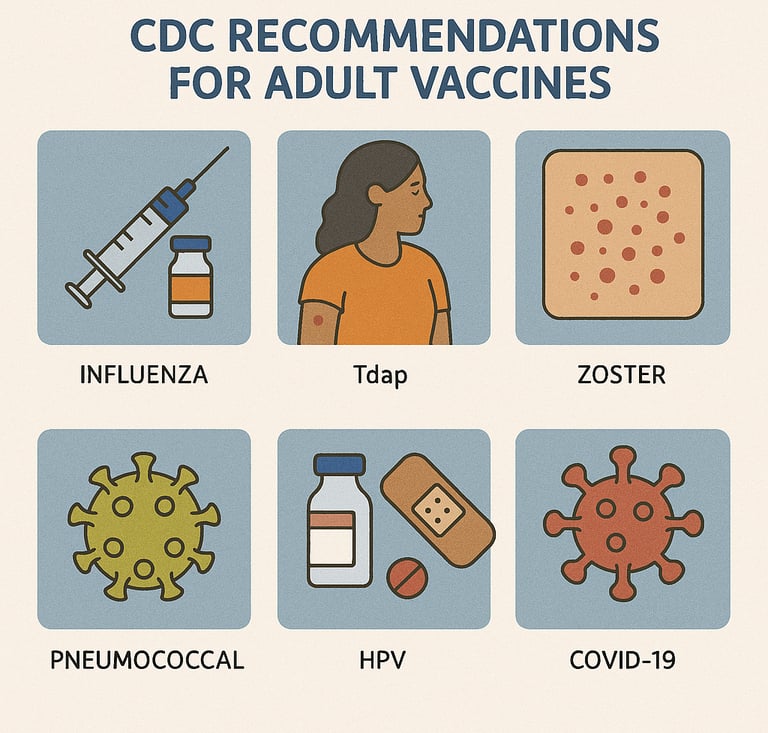
Q2: Which vaccines are recommended for all adults?
A: According to CDC guidelines:
Flu (influenza): Every year
COVID-19: Stay up to date with current CDC recommendations
Tdap (tetanus, diphtheria, pertussis): One dose as an adult, then Td or Tdap booster every 10 years
Q5: Can adults catch up on missed vaccines?
A: Yes. Adults who missed childhood vaccines or don’t know their vaccine history can safely receive catch-up vaccines. A healthcare provider can review medical history and recommend what’s needed.
Q3: Which vaccines are based on age?
Shingles (Shingrix): Age 50 and older (2-dose series)
Pneumococcal vaccine: Age 65 and older (or younger if chronic conditions or weakened immune system)
Sciatica: Questions & Answers
Q1: What is sciatica?
A: Sciatica is pain that radiates along the path of the sciatic nerve, which runs from the lower back through the hips, buttocks, and down each leg. It usually affects only one side of the body.
Q2: What are the symptoms of sciatica?
A: Common symptoms include:
Sharp, shooting pain from the lower back into the leg
Burning, tingling, or numbness in the leg or foot
Muscle weakness in the affected leg
Pain that worsens with sitting, coughing, or sneezing
Q4: Is sciatica dangerous?
A: Most cases are not dangerous and improve with time. However, urgent medical care is needed if sciatica is accompanied by:
Loss of bladder or bowel control
Severe or progressive leg weakness
Sudden, severe pain after trauma
Q3: What causes sciatica?
A: Sciatica is usually caused by pressure or irritation of the sciatic nerve due to:
Herniated or bulging disc in the spine
Bone spur (extra bone growth)
Spinal stenosis (narrowing of the spinal canal)
Muscle spasm or injury
Rarely, tumors or more serious conditions
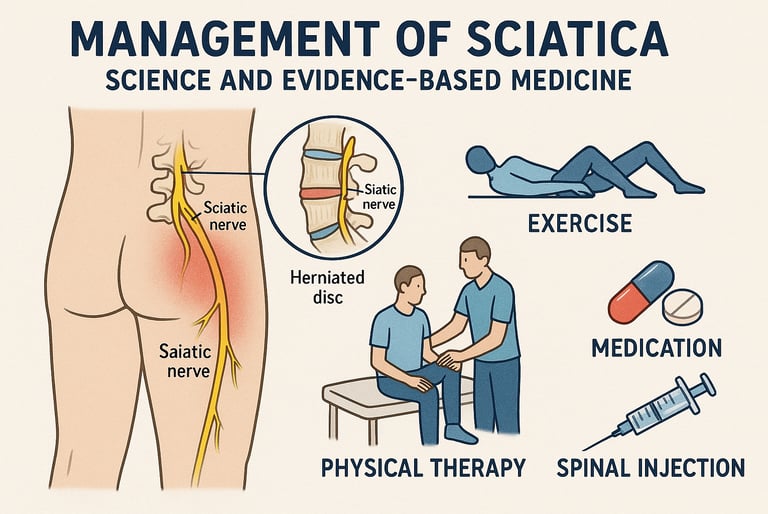
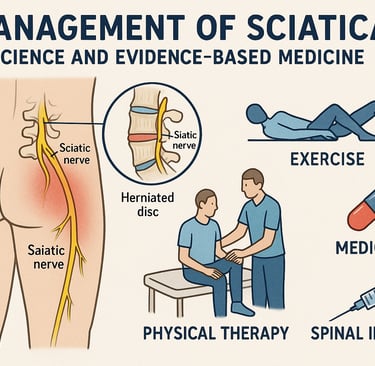
Q5: How is sciatica treated?
A:
Self-care: Rest, gentle stretching, heat/ice, over-the-counter pain medicine
Medical care: Prescription medicines, physical therapy, steroid injections
Surgery: Considered for severe, persistent cases not improving with other treatments, or if there is nerve damage
Prevention: Good posture, core-strengthening exercises, maintaining a healthy weight
Seasonal Allergy: Questions & Answers
Q1: What are seasonal allergies?
A: Seasonal allergies, also called hay fever or allergic rhinitis, occur when the immune system overreacts to pollen from trees, grasses, or weeds. They typically flare up during certain times of year (spring, summer, or fall).
Q4: Are seasonal allergies dangerous?
A: Seasonal allergies are not life-threatening but can:
Interfere with sleep, school, or work
Make asthma worse
Cause frequent sinus infections or ear infections in some people
Q2: What are the symptoms?
A: Symptoms may include:
Sneezing
Runny or stuffy nose
Itchy eyes, nose, or throat
Watery, red eyes
Fatigue or poor sleep
Coughing or post-nasal drip
Q6: What can I do at home to reduce symptoms?
Keep windows closed during high pollen days
Shower and change clothes after being outdoors
Use air filters or purifiers indoors
Try daily nasal irrigation with sterile saline
Wear sunglasses outdoors to reduce eye exposure
Q3: What causes seasonal allergies?
A: Seasonal allergies are caused by exposure to pollen. The immune system mistakenly treats pollen as harmful, releasing histamine and other chemicals that cause allergy symptoms.
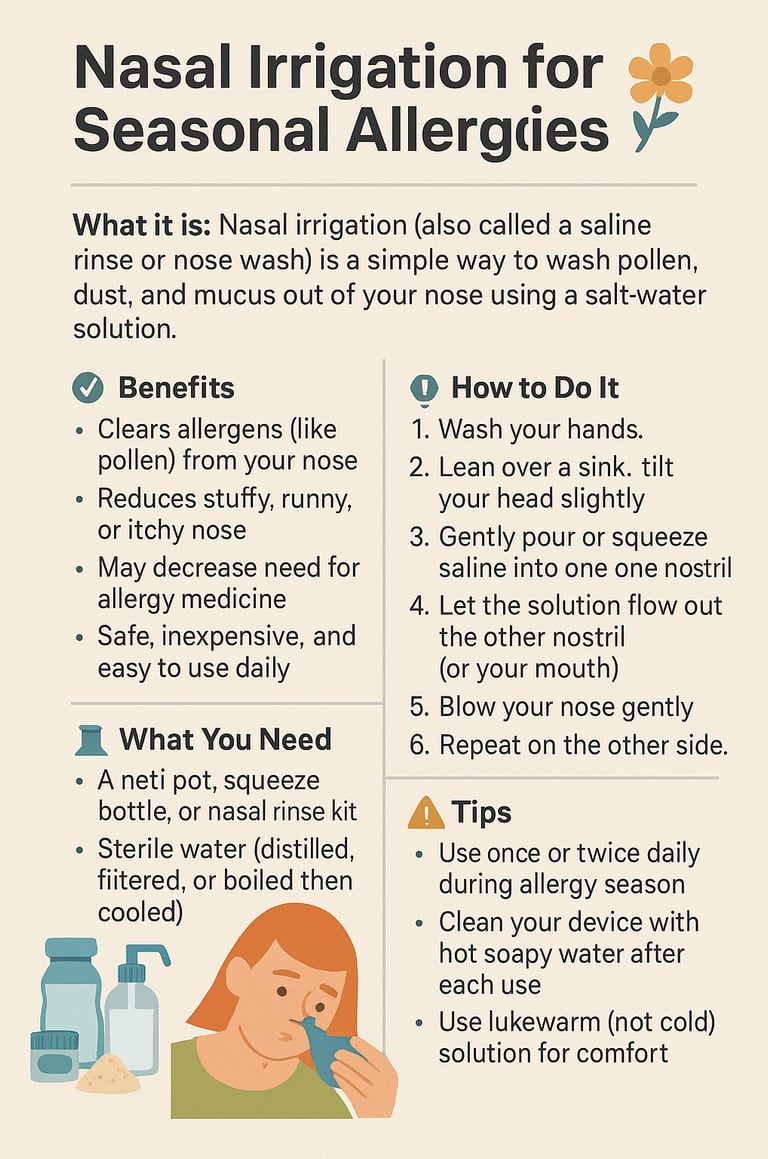
Q5: How are seasonal allergies treated?
A: Treatment focuses on reducing exposure and controlling symptoms:
Avoiding triggers: Keep windows closed, shower after being outdoors, use air filters
Medications: Antihistamines, decongestants, nasal steroid sprays, eye drops
Allergy shots (immunotherapy): For severe cases not controlled by medicines
Lifestyle: Wearing sunglasses, washing bedding often, limiting outdoor time during high pollen counts
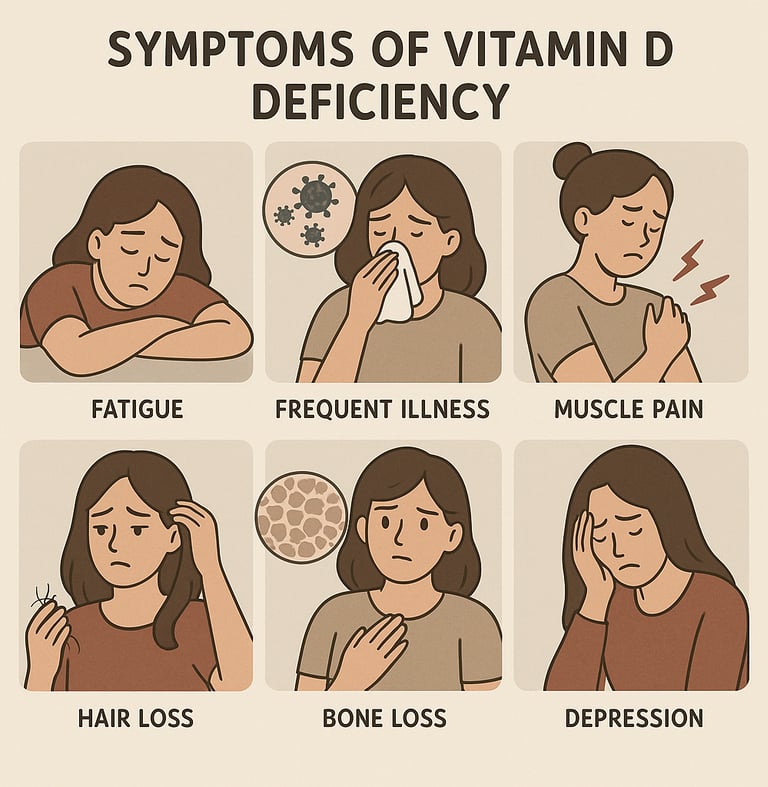
Vitamin D Deficiency: Questions & Answers
Q1: What is vitamin D deficiency?
A: Vitamin D deficiency means the body doesn’t have enough vitamin D, a nutrient that helps absorb calcium and keep bones, muscles, and the immune system healthy.
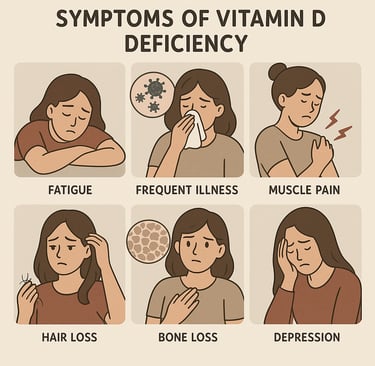
Q2: What are the symptoms of vitamin D deficiency?
A: Many people have no obvious symptoms, but signs can include:
Fatigue or low energy
Bone or muscle pain
Muscle weakness or cramps
Increased risk of infections
Slow wound healing
In severe cases: soft or weak bones (rickets in children, osteomalacia in adults)
Q4: Why is vitamin D important?
A: Vitamin D helps the body absorb calcium and maintain strong bones. Without enough, people are at risk of osteoporosis, fractures, falls, and possibly weakened immunity and chronic health problems.
Q3: What causes vitamin D deficiency?
A: Causes include:
Not enough sunlight exposure
Diet low in vitamin D (few fortified foods, little fatty fish or dairy)
Darker skin (less vitamin D made from sunlight)
Aging (skin makes less vitamin D)
Medical problems (obesity, kidney or liver disease, digestive disorders like celiac or Crohn’s)
Certain medications (steroids, anticonvulsants)
Q5: How is vitamin D deficiency treated?
A: Treatment may include:
Supplements: Vitamin D tablets, capsules, or drops (dose guided by a doctor)
Diet: Eating foods rich in vitamin D (fatty fish, fortified milk, eggs)
Sunlight: Safe exposure to sunlight can boost vitamin D production
Treating underlying conditions: Managing diseases that affect absorption or metabolism
Thyroid Disease: Questions & Answers
Q1: What is the thyroid and what does it do?
A: The thyroid is a small, butterfly-shaped gland in the neck. It makes thyroid hormones, which control metabolism—how the body uses energy. These hormones affect heart rate, digestion, weight, mood, and temperature regulation.
Q2: What are the main types of thyroid disease?
A: The most common thyroid disorders are:
Hypothyroidism: The thyroid makes too little hormone (slow metabolism).
Hyperthyroidism: The thyroid makes too much hormone (fast metabolism).
Goiter: Enlargement of the thyroid gland.
Thyroid nodules: Lumps in the gland, usually benign but sometimes cancerous.
Thyroid cancer: Rare, but treatable, especially if found early.
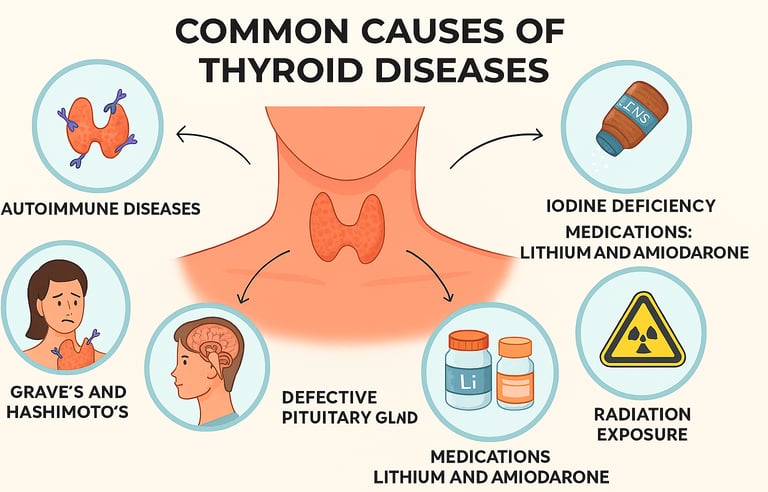
Q4: What causes thyroid disease?
A: Causes include:
Autoimmune disease: Hashimoto’s thyroiditis (hypothyroidism) or Graves’ disease (hyperthyroidism)
Iodine deficiency or excess
Medications: Lithium, amiodarone
Radiation exposure
Genetics or family history
Thyroid surgery or treatments
Q3: What are the symptoms?
A:
Hypothyroidism (underactive thyroid): Fatigue, weight gain, cold intolerance, constipation, dry skin, hair loss, depression, slow heart rate.
Hyperthyroidism (overactive thyroid): Weight loss, rapid heartbeat, sweating, anxiety, tremors, frequent bowel movements, heat intolerance.
Goiter or nodules: Visible swelling in the neck, trouble swallowing or breathing (if large).
Q5: How is thyroid disease treated?
A: Treatment depends on the type:
Hypothyroidism: Thyroid hormone replacement (levothyroxine)
Hyperthyroidism: Medications (antithyroid drugs), radioactive iodine, or surgery
Goiter/nodules: Monitoring, medication, or surgery if large or cancerous
Thyroid cancer: Surgery, radioactive iodine, and sometimes hormone therapy
Sexually Transmitted Diseases (STDs): Questions & Answers
Q1: What are STDs?
A: Sexually transmitted diseases (STDs), also called sexually transmitted infections (STIs), are infections spread mainly through sexual contact (vaginal, oral, or anal sex). Some also spread through blood, shared needles, or from mother to baby during pregnancy or birth.
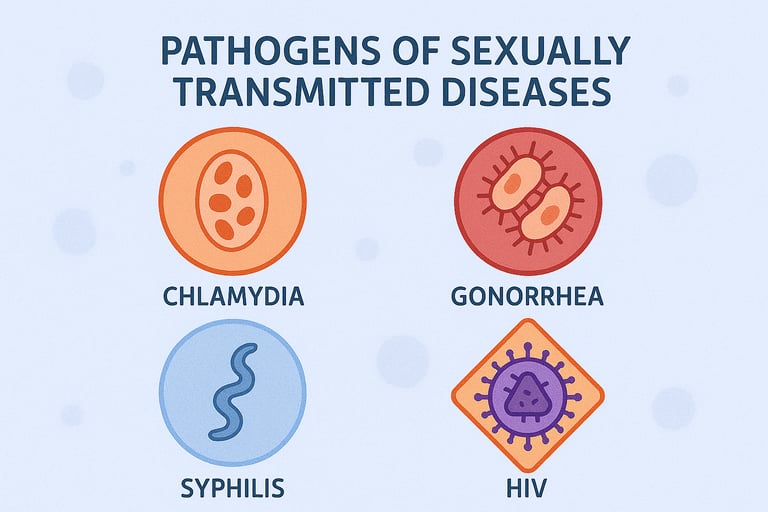
Q2: What are the most common STDs?
A: The most frequently seen STDs in primary care include:
Chlamydia
Gonorrhea
Syphilis
HIV (Human Immunodeficiency Virus)
HPV (Human Papillomavirus)
Trichomoniasis
Q3: What are the symptoms of STDs?
A: Many STDs cause no symptoms at first. When symptoms occur, they may include:
Genital sores, blisters, or warts
Unusual vaginal or penile discharge
Pain or burning with urination
Pelvic pain or pain with sex
Rash, swollen glands, or flu-like symptoms
Because they are often silent, regular screening is essential.
Q4: Are STDs dangerous?
A: Yes—if untreated, STDs can cause:
Infertility (chlamydia, gonorrhea)
Pregnancy complications and risks to newborns
Chronic pain (pelvic inflammatory disease)
Neurologic disease, blindness, or organ damage (syphilis)
Increased risk of HIV transmission
Certain cancers (HPV causes cervical, anal, throat cancers)
Q5: How are STDs treated or prevented?
A:
Treatment:
Curable: Bacterial (chlamydia, gonorrhea, syphilis) and parasitic (trichomoniasis) infections with antibiotics/antiparasitics
Not curable but controllable: Viral STDs (HIV, herpes, HPV)
Prevention:
Consistent condom use
Regular STD screening and partner testing
Vaccines for HPV and hepatitis B
Avoiding needle sharing
Practicing mutual monogamy
Chlamydia
What is it?
A common bacterial STD, often silent but easily treated
Why it matters:
Can cause pelvic inflammatory disease and infertility if untreated.
Treatment:
Cured with antibiotics.
Both partners should be treated.
Prevention:
Condom use, regular screening, treating both partners.
Trichomoniasis
What is it?
A parasitic infection spread through sex.
Why it matters:
Can increase risk of HIV transmission
Causes pregnancy complications
Treatment:
Easily cured with a single antibiotic dose (metronidazole or tinidazole).
Prevention:
Condom use, treat both partners.
Gonorrhea
What is it?
A bacterial STD that can infect the genitals, throat, or rectum.
Why it matters:
Can cause infertility, pelvic inflammatory disease, or spread to blood/joints.
Treatment:
Antibiotics (resistance is common, so treatment must be guided by a doctor).
Prevention:
Condom use, regular testing, treat both partners.
Syphilis
What is it?
A bacterial STD with stages: sore → rash → hidden → organ damage.
Why it matters:
Very dangerous if untreated, but curable in early stages.
Treatment:
Penicillin injection cures syphilis at all stages.
Prevention:
Condom use, regular testing, early treatment for partners.
HPV (Human Papillomavirus)
What is it?
A very common virus; some types cause genital warts, others cause cancers.
Why it matters:
Can cause cervical, anal, and throat cancers.
Treatment:
No cure for virus itself.
Warts can be treated/removed.
Regular Pap smears detect precancerous changes.
Prevention:
HPV vaccine (very effective)
Condom use lowers risk
HIV
What is it?
A viral infection that weakens the immune system.
Symptoms:
Early: flu-like illness
Later: weight loss, infections, night sweats
May be silent for years
Why it matters:
Untreated HIV leads to AIDS.
Increases risk of severe infections and cancers.
Treatment:
No cure, but lifelong antiretroviral therapy (ART) keeps virus under control.
Prevention:
Condom use, regular testing, PrEP (preventive medicine), never sharing needles.
Disclaimer
For educational purposes only. Not medical advice. No physician-patient relationship established.
In emergencies, call 911.
Copyright
© 2025, David He, MD, PhD, All rights reserved.